DVT (Deep Venous Thrombosis) | Austin TX
Definition of Deep Venous Thrombosis (DVT)
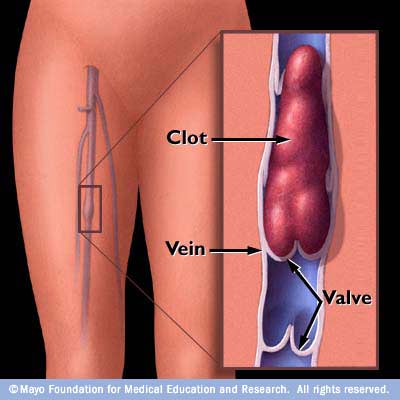
DVT, or Deep Venous Thrombosis , is the formation of blood clots (also known as thrombus) within the deep veins of the body. The most common locations are the legs, followed by the pelvis, although they can occur at any location of the body. DVT is a relatively common medical condition, affecting up to 600,000 Americans each year. Over 1 million people undergo evaluation for DVT annually in the United States.

Symptoms of DVT
At least 50% of those with deep venous thrombosis have no symptoms at all and the condition is discovered by imaging studies alone. Symptoms of deep venous thrombosis / DVT include pain, swelling (also known as edema), skin discoloration (red, pink, purple, blue, or tan), tenderness of the leg, enlarged or engorged veins, increased warmth of the skin, and “tightening” of the skin.
Other symptoms can be related to the clot floating in the body and getting lodged in the lung tissue, an episode referred to as pulmonary embolism or PE. A pulmonary embolism can cause sudden chest pain, shortness of breath, cardiac arrhythmia, and even sudden death.
Cause of Deep Venous Thrombosis
The etiologies of deep venous thrombosis are multiple. They include prolonged immobilization (such as during prolonged travel), surgery, physical trauma, pregnancy, medications such as hormone therapy and birth control medications, obesity, cancer, genetic or inherited clotting disorders, vein catheters, May-Thurner Syndrome, advanced age, and infections. The cause of many episodes of DVT is not determined or idiopathic.
Some known predisposing factors that lead to the veins clots forming include decreased blood flow within the veins (i.e. venous stasis), damage to the blood vessel walls and the valves located within the vein walls, and thickening of the blood itself (known as hypercoagulability).
Diagnosis of DVT
The most common way that DVT is diagnosed is through a vein ultrasound, also known as a venous duplex study. Another common way they are diagnosed is with a special type of blood test referred to as a D-dimer test. Other methods of diagnosis of deep venous thrombosis include CT scan (CAT scan), MRI, and catheter venography. Physical exam by a doctor can aid in the diagnosis, but a confirmatory imaging test or blood test is always necessary. Please contact the ultrasound department of our vascular center at (512) 339-9102 to get a vein screening performed or to speak with our physician. Walk-in appointments are welcome.
Complications of DVT
The most dangerous complication related to DVT is the clot spreading or traveling to another location of the body. If the clot dislodges and floats to the heart and lungs, it can lead to a Pulmonary Embolism (PE) than can be lethal.
Post-thrombotic Syndrome (PTS) is a chronic condition that occurs as the result of deep venous thrombosis. Post-thrombotic syndrome occurs when the veins become damaged long-term as a result of scar tissue formation or valve damage within the lining of the veins. This can lead to areas of obstruction or stenosis that hinders the ability of blood to circulate normally. If the valves are dysfunctional within the veins, this can lead to venous insufficiency or venous reflux, a chronic circulatory disease. This often is referred to as “venous hypertension” of the leg. The symptoms of this condition include long-term leg swelling / edema, chronic leg pain that is often worse with walking or prolonged standing, skin damage that often manifests as brown discoloration at the ankles, or skin ulcers of the leg (most often located on the inside of the ankles).
Treatment of Deep Venous Thrombosis
There are many different treatment options available for deep venous thrombosis / DVT. The type of treatment offered by your physician often depends on the location and severity of the clots. The most common treatment offered for deep venous thrombosis is anticoagulant medications, which includes Coumadin (Warfarin), Xarelto, Eliquis, Lovenox, Heparin, Argatroban or a combination of these. Some of these medications have been more extensively researched in regards to DVT treatment. The most common length of treatment for the initial diagnosis of DVT blood clots is three to six months of blood thinner medications. For an episode of pulmonary embolism, the length of treatment is at least 6 months and a pulmonologist consult may also be indicated. Patients with recurrent DVT blood clots may require life-long anticoagulation medications. The best options for treatment is best determined by your doctor based on your particular circumstance and your underlying medical conditions.
When these anticoagulant medications cannot be administered for medical reasons (such as risk of bleeding), a metal filter device is often placed within the vein (known as an Inferior Vena Cava Filter or IVC filter). IVC filters can often be removed at a future date when they are no longer needed.
Other common therapies for DVT include “clot-busting” or “clot-dissolving” medications that can be delivered through a catheter directly into the clot under x-ray guidance. One such medicine is referred to as t-PA or Tissue Plasminogen Activator. These medications can only be administered in a hospital setting. These medications are often administered in addition to the other anticoagulants above in order to more quickly and effectively resolve the clot.
The use of t-PA has been associated with better long-term outcomes in patients with extensive DVT. The use of t-PA can significantly decrease the risk of long-term dysfunction of the affected arm or leg (chronic pain, chronic swelling, or other post-thrombotic syndrome complications), especially in patients with iliac vein and femoral vein DVT. Patients with upper leg or pelvic vein DVT should be assessed by a vascular surgeon for possible t-PA administration. Also, patients with arm DVT should also be assessed for possible t-PA if thoracic outlet syndrome is suspected. The sooner that t-PA can be administered after a DVT is diagnosed the better, as better clot resolution can be achieved in the short-term. The longer that a DVT is present in an extremity the more scar tissue develops in the clot and in the vein, and the harder it tends to be to dissolve the clot with t-PA. Therefore the timing of t-PA administration is critical.
If a DVT is subacute or chronic (i.e. has been present for weeks, months, or years) and is leading to persistent symptoms in an arm or leg, there is still often some hope of successful outcomes with interventional therapies. Often venography with angioplasty or stenting can be successful. Vein obstruction or stenosis that do not respond to anticoaglunt medications do often respond to balloon angioplasty or stents placed into the vein under x-ray guidance. Imaging studies of the area of clot can help determine if you are a candidate for such therapy. CT venography and MR venography can both be extremely useful.
It is best to have a consultation with a board-certified Vein Specialist / Vascular Surgeon as quickly as possible after being diagnosed with a DVT so that all of your options can be discussed. Contact our Vascular Center at (512) 339-9102 to arrange a consultation.
Prevention of DVT
Preventative measures are advised for at risk medical, surgical, and pregnant patients. Prophylaxis includes early and frequent exercise / movement, compression stockings, pneumatic compression devices, avoiding prolonged sitting without movement, maintaining normal body weight, and blood-thinner medications such as heparin and Lovenox. Genetic testing or blood / hematology testing may be indicated to evaluate for an underlying blood disorder that may predispose individuals to blood clots. The results of this testing may alter the recommendations for treatment, including the type of medication to administer and the length of treatment. Please consult with a vascular physician specialist to find out which options are best for your particular situation.