Varicose Veins Austin, TX | Leg Vein Removal Experts | Vein Specialists
Varicose Veins & Spider Veins
To learn more about varicose veins, visit our official Vein & Laser Center webpage HERE.

Varicose Veins
Veins are blood vessels that return blood to the heart once it has circulated through the body (as opposed to arteries, which carry oxygen-rich blood from the heart to the body). Healthy veins carry the non-oxygenated blood back to the heart and lungs so that the blood cells can be replenished with oxygen, allowing the refreshed blood to be reenter the circulation once again. Veins have one-way valves that help keep blood flowing in the proper direction (i.e. toward the heart).
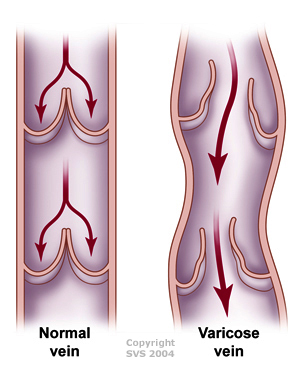
If these vein valves stop functioning in the way that they are supposed to, blood begins to flow backwards and pool in the veins, raising the blood pressure in the veins themselves. This process leads to a vein disease called venous hypertension and venous reflux disease. The build-up of pressure within the diseased veins leads to the vein walls stretching and thinning. This process leads to the development of unsightly enlarged and bulging veins beneath the surface of the skin. These abnormal stretched and enlarged veins are known as varicose veins.
Varicose veins are swollen, dark blue or purple blood vessels that you can obviously see and feel beneath the skin. They often look like twisted cords, and usually appear on the calves, inside of the legs, and ankles. As varicose veins continue to weaken under the constant strain, they often continue to get bigger and balloon outward. This tends to raise the skin surface and causing the skin to bulge and thin out or get discolored.
Patients with varicose veins often develop aching, throbbing, cramping, burning, itching and other symptoms that may indicate a need for medical attention. Other patients with varicose vein disease may remain without symptoms for years.
Varicose veins are considered a “disease” since the valves within the veins are defective and the blood flow within these veins is backwards. The disease process does tend to spread to other areas of the legs over time, as the leg veins are connected to one another through a series of branch connections. These vein connections allow the venous hypertension to spread from diseased varicose veins to healthy vein segments. It is often described as a “domino effect” of more and more vein valves breaking as they are exposed to the elevated vein pressure from adjacent diseased veins. Therefore, varicose vein disease does tend to worsen over time and begins to involve larger and larger areas of the leg. The sooner the condition is treated, the easier it is to deal with medically.

Typical Appearance of a Varicose Vein
Risks Factors For Varicose Veins
While varicose veins can affect nearly anyone of any age, they tend to occur more often in patients possessing certain risk factors, including:
- Occupations with prolonged standing
- Family history of varicose veins
- Older age
- Pregnancy, especially multiple pregnancies
- Obesity / being overweight
- Trauma to the legs or prior blood clots in the legs
- Heredity / genetic predisposition
- Gender (females more prone then males)
Although the risk tends to increase with age, varcicose vein are often seen at very young ages, even in the teenage years.
Diagnosing Varicose Veins
Your doctor can usually diagnose varicose veins and any associated venous conditions after a physical examination of the affected area. Additional testing may also be required, such as a venous duplex ultrasound or venous reflux study. These studies allow the physician to obtain an anatomical “road map” of your circulation. This allows for more precise and targeted treatment options.
When to Consider Treatment
If varicose veins are leading to any symptoms, one should consider medical evaluation. Patients report a wide variety of symptoms including burning or aching pain, throbbing, itching, and pressure sensations. Leg or ankle swelling is also a prominent complaint in those with varicose vein disease. Both discomfort and swelling can be signs of significant underlying circulation issues such as venous reflux which requires additional testing for diagnosis.
While many of those suffering with varicose veins may not have leg discomfort, many patients with varicose veins are bothered by their appearance. Cosmetic reasons alone are the most common reason patients seek treatment for varicose veins and spider veins.
Patients often report embarrassment and reluctance to wear shorts or skirts. The condition can lead to avoidance of social activities or sports or the eroding of one’s self-confidence. They can even be the root of psychological problems related to body perception such as body dysmorphic disorder.
Long-standing varicose vein disease can lead to many different problems, some more serious than others. The problems that can arise over time include chronic wounds or ulcers in the feet and ankles (e.g. venous stasis ulcers), chronic leg or foot swelling or edema, discoloration or darkening pigment changes in the skin, thinning of the skin or other severe skin disorders including stasis dermatitis, recurrent thrombophlebitis, and increased risk of skin infections such as cellulitis. The longer that the varicose vein disease is present, the higher the likelihood of developing these more complicated medical issues.
Pain or discomfort symptoms in the legs can also be the signs of more serious underlying medical conditions in the veins as well. Both phlebitis / thrombophlebitis as well as deep venous thrombosis can lead to pain or swelling in the veins of the leg. These conditions are best diagnosed by physician through a physical exam and vein ultrasound study.
Treatment of Varicose Veins
There are many reasons people seek treatment for varicose veins, including frequent discomfort, chronic swelling / edema, or skin damage. Many people with venous disease also seek cosmetic treatment to eliminate or reduce the appearance of unsightly varicose or spider veins on their legs. Sometimes patients seek out treatment to reduce their chances of developing more significant circulation problems down the road if their veins are left untreated.
There are several treatment options available to eliminate or reduce the appearance of veins and relieve any symptom. These therapies may include self-care methods such as losing weight, keeping the legs elevated, using over-the-counter anti-inflammatory medications, regular exercise, and wearing compression stockings.
More immediate and permanent relief is often achieved through interventional therapies. With advancements in technology, vein treatments can be administered with minimal discomfort and very fast recovery. Some of the more common and effective therapies include sclerotherapy injections, laser therapy, and catheter based treatments. The vein procedures described below are typically performed in our vein clinics, with immediate discharge afterwards.
- Sclerotherapy treats varicose veins by injecting a solution into the targeted veins that causes them to gradually disappear. The sclerosing solution used during the procedure irritates the vein lining and turns it into scar tissue that eventually fades away. The therapy is typically done under image guidance with ultrasound. Foam sclerotherapy is the most commonly method. Depending on the extent of your disease, it may require several treatment sessions to achieve the desired result.
- Endovenous laser therapy (EVLT) is a minimally invasive laser procedure that treats varicose veins faster, safer and more effectively than surgical procedures, as it precisely targets the affected veins with a laser probe under ultrasound guidance. The laser energy delivered to the vein causes the vein walls to scar shut so that blood can no longer flow through them. Following laser vein therapy, the venous blood flow that once circulated through the varicose veins is diverted into healthy veins.
- Radiofrequency vein ablation (Venefit ClosureFast procedure) is a minimally invasive catheter procedure that is done through an IV that treats varicose veins safer and more effectively than surgery, as it precisely targets the affected veins with a radiofrequency probe under ultrasound guidance. The radiofrequency energy delivered to the veins causes the vein walls to scar shut so that blood can no longer flow through them. Following radiofrequency ClosureFast vein therapy, the venous blood flow that once circulated through the varicose veins is diverted into healthy veins.
- Varithena Endovenous Chemical Ablation (ECA) is a minimally invasive procedure that is often used to treat very tortuous or serpentine varicose veins and saphenous veins of the legs. The Varithena medication that is utilized is FDA approved for the use in venous reflux disease of saphenous veins in the legs. Varithena is also approved for the use of tortuous blue bulging varicose veins that are visible beneath the surface of the skin. This therapy has significantly diminished the need to undergo vein stripping surgery or phlebectomies. It allows surface varicose veins to be closed without having to remove then with surgery.
- Clarivein endovenous ablation is a minimally invasive procedure that is utilized to treat venous insufficiency in the legs that is leading to the development of varicose veins. Unlike thermal varicose vein therapies that utilize laser or radiofrequency heat to close abnormal veins, Clarivein uses a unique rotating catheter that closes the abnormal veins with rotational mechanical energy. The rotating catheter delivers a sclerosant drug to the vein wall while it is spinning, causing almost immediate vein closure. Since no heat is utilized, the Clarivein treatment can be safely utilized on veins that are close to important nerves that provide sensation to the skin. The most common area that the Clarivein device is utilized in our vein center is with varicose vein disease below the knee, where important nerves might otherwise be at risk if using other technologies.
- Micro-phlebectomy, or just “phlebectomy,” is a traditional vein plastic surgery that has been utilized for many decades to treat leg varicose veins. After first numbing the leg with local anesthetic, small micro-incisions are placed over the veins in order to surgically remove them. A small specialized instrument is utilized to physically remove the veins through the small incision sites. Although this is more invasive than the other therapies described, it is very effective for larger varicose veins. Micro-phlebectomy is usually performed in the clinic rather than the hospital, although if deeper anesthetic is desired it can be done in a surgery center.
- VenaSeal medical glue is s minimally-invasive method to treat leg varicose veins. The benefits of this procedure over other treatments is that is only involves a single IV stick, is associated with less discomfort than other therapies, it does not require any activity or exercise limitations afterwards, and it does not require the use of post-procedure compression stockings. VenaSeal is the newest of the FDA approved therapies available.
For more information regarding treatment options, please refer to the Treatment of Varicose Veins page of our website.
Preventing Varicose Veins
While there is no surefire way to prevent varicose veins from developing, there are certainly life changes that can be made in order to reduce your risk of developing further problems with this condition. This may include:
- Exercising regularly
- Maintaining a healthy weight
- Eating a diet high in fiber and low in salt
- Elevating the legs
- Avoiding sitting or standing in one position for too long
Your doctor will provide you with more information as to how you can reduce your risk of varicose veins and maintain strong vascular health.
Spider Veins
Spider veins, also known as telangiectasias, are small, thin blood vessel clusters that are easily visible within the skin. They are often red, pink, or purple and are usually dispersed as clusters in certain locations of the body. They appear most commonly on the legs, but may be seen anywhere on the body, including the face. They typically have the appearance of a series of lines, tree branches or a spider- web-like shape (hence the name). They tend to be much smaller than varicose veins, somewhere in the range of size of a small thread or at most a toothpick. It is very common for people to seek out cosmetic therapies to rid their skin of these unsightly veins. While most cases of spider veins are of purely cosmetic concern, some patients may also experience uncomfortable symptoms such as aching, burning, swelling, itching, and cramping from this condition.
Many patients are bothered by the appearance of spider veins on prominent areas of their bodies such as the legs or face, and seek treatment to restore a smooth, clear appearance. Many of these treatments are highly effective and minimally invasive, offering aesthetically-pleasing results without painful or lengthy downtimes.

Typical Appearance of Spider Veins
Causes of Spider Veins
Spider veins develop as a result of a backup of blood in certain veins, which may occur when the valves in the veins cannot effectively keep blood from flowing backwards as it moves up the legs. As blood collects in the vein, it begins to expand and becomes visible under the surface of the skin or within the skin itself.
Spider veins are common in the legs because of the fact that blood flow must work against gravity to travel back up to the heart, with the legs having to carry the largest burden of gravitary blood flow. This condition affects nearly half of all adults over the age of 50 in the US, and may occur as a result of hormonal changes, pregnancy, obesity, trauma, sun exposure and genetic predisposition. You are much more likely to develop spider veins is you have immediate relatives with the same condition.
Your doctor can diagnose spider veins through a physical examination and will determine an appropriate treatment method based on a thorough evaluation of your condition and medical history. An ultrasound may be performed to evaluate the severity of the condition and identify the underlying cause to ensure the most effective treatment approach.
Treatment of Spider Veins
There are several minimally-invasive aesthetic treatment options available to eliminate the appearance of spider veins and allow patients to once again proudly show off their legs. Newer treatment options offer patients few side effects, less pain and shorter recovery times than traditional vein removal procedures.
One of the common and standard treatments for spider veins is sclerotherapy. Sclerotherapy involves injecting a sclerosant solution directly into the affected veins, causing them to gradually disappear. This procedure is typically performed in the doctor’s office and takes less than an hour. Depending on the extent of their vein disease, patients may require one to four treatment sessions in order to achieve their desired result. Additional treatment options for spider veins may include surface laser therapy, in which thermal energy delivered to the skin is used to eliminate the veins.
Mild cases of spider veins may also be treated with compression stockings to put pressure on the veins and promote normal blood flow. Thermal therapies such as laser therapy, Ohmic thermolysis, Veinwave, or VeinGogh devices may also be potential options. Your doctor will discuss with you what he feels are the best options for treating your condition based on your desires and expectations.
For more information regarding treatment options, please refer to the Treatment of Spider Veins page of our website.
Prevention of Spider Veins
While there is no sure way to prevent spider veins from developing, there are certainly life modifications that can help reduce the risk of developing this unsightly condition. These include losing weight, exercising regularly, wearing support hose / stockings, and wearing comfortable / supportive shoes. It is important to move the legs frequently, especially if your job requires long periods of sitting or standing in one place. Your doctor will provide you with specific guidelines to effectively reduce the risk of spider veins so that you can maintain beautiful and youthful appearing legs for many years.