Peripheral Artery Disease | Austin TX
Peripheral Artery Disease (PAD) of the Legs
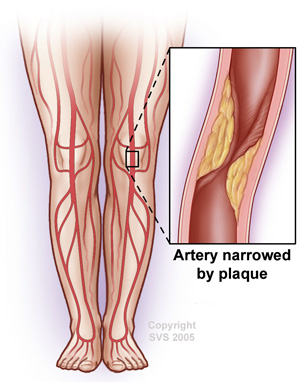
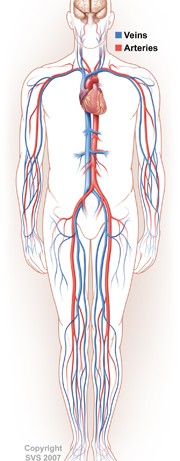
Peripheral artery disease, also referred to as peripheral vascular disease, is a serious vascular condition involving a buildup of plaque within the peripheral arteries of the legs and feet. There are multiple other medical terms used to describe this abnormal plaque build-up, including the terms “hardening of the arteries,” atherosclerosis, arteriosclerosis, PAD, or PVD. The diseased artery plaque is made up of fat, cholesterol, calcium, fibrous tissue, and other substances from within the blood. It can accumulate as a result of several different factors, often accelerated by aging, smoking, diabetes, and high blood cholesterol or triglycerides. The buildup of plaque can severely narrow or block the arteries and limit the flow of oxygen-rich blood to your body.
Peripheral artery disease can lead to pain in the legs, either at rest or sometime only during walking (a symptom called claudication). It can also lead to wounds or ulcers on the legs or feet, poor wound healing, infections in the legs or feet, coldness or numbness of the legs and feet, and neuropathy type symptoms. In severe cases it can lead to gangrene and amputation of the toes, foot, or even amputation of the leg. Atherosclerotic plaque build-up often involves the legs, but can also affect the other arteries that carry blood from your heart to your head, arms, kidneys, stomach, and other organs. Atherosclerotic disease can often affect the heart itself, leading to heart attacks, as well as the carotid arteries, leading to strokes. Patients who are diagnosed with PAD should therefore also be screened for arterial disease in other parts of their body, including the coronary arteries and carotid arteries.
Fortunately, there are several treatment options available to relieve symptoms and prevent the disease from further progressing, including lifestyle changes, smoking cessation, medications, and minimally invasive treatments. If you arrange a consultation at Austin Vascular Surgeons, Dr. Gotvald will discuss these various options with you to determine the most effective treatment for your individual condition.
Causes and Risk Factors for PAD
Peripheral artery disease develops as a result of atherosclerosis, which is a buildup of plaque within the arteries that narrows the vessel and restricts blood flow. PAD is also referred to as hardening of the arteries of the legs. It is most common in elderly patients with other medical conditions, such as diabetes, high cholesterol, high triglycerides, high blood pressure / hypertension, kidney disease, and heart disease, as well as those with a family history of these conditions. Other patients may be at a higher risk for developing PAD, including those who:
- Are Smokers or have smoked cigarettes or cigars in the past
- Are obese
- Are over the age of 50
- Do not exercise regularly
It is important for these patients to take certain precautions to reduce their risk of PAD and other serious conditions. It is also important for those with risk factors to get the appropriate screening studies performed by a vascular specialist in order to check for the disease.
Symptoms of PAD
Many patients with peripheral artery disease do not experience any symptoms and may not be aware that they have this condition, while others may experience:
- Pain or cramping in the hips, thighs, calves, or feet (especially during walking)
- Numbness, tingling or weakness in the legs or feet
- Skin sores or ulcers on the legs or feet
- Hair loss
- Weak pulses in the legs or foot
- Coldness in the leg or foot
- Gangrene in the toes, foot, or leg
- Infections such as cellulitis or osteomyelitis (bone infection) in the legs or feet
Symptoms can vary significantly between patients, so it is important to see a knowledgeable vascular specialist in order to accurately diagnose this condition and to make appropriate recommendations for treatment and follow-up.
Diagnosis of PAD
Most cases of peripheral artery disease can be effectively diagnosed in a physicians office using a test called an Ankle Brachial Index (ABI), which compares blood pressure in your ankle to blood pressure in your arm to show how well blood is flowing in your limbs. This study uses specialized blood pressure cuffs attached to your legs and feet that measure blood flow with the assistance of a computer. ABIs are often performed as a screening test for PAD, but can also be used to determine the severity of the vascular disease or follow the progress of the disease. A pre-exercise and well as post-exercise test is sometimes necessary, depending on your specific vascular condition. The ABI is then often followed up by an artery doppler ultrasound test, which uses harmless sound waves to trace the flow of blood within your blood vessels to determine any areas of blood vessel narrowing or occlusion. While these tests can typically determine whether or not there are blood flow problems within the legs, it may not always be able to determine which specific blood vessels are affected or how long the blockages really are. Additional testing to determine the specific blood vessels affected by this disease may include an angiography, which involves injecting a contrast dye into the bloodstream to watch blood flow through X-ray imaging assistance. Your doctor may also wish to perform certain blood tests, CT angiogram (CTA), or magnetic resonance angiogram (MRA) to gain additional information about your vascular disease.
Treatment of PAD
Treatment for peripheral artery disease aims to relieve symptoms and stop the progression of the disease to reduce the risk of serious complications. Patients with mild forms of PAD may be able to effectively treat their condition through life changes, such as quitting smoking, eating a healthy, balanced diet and following a regular exercise plan. It is also important for patients, especially those with diabetes, to take good care of their feet. Your doctor may also prescribe medications to treat PAD, including those designed to:
- Lower cholesterol
- Lower high blood pressure
- Control blood sugar
- Prevent blood clots
- Relieve pain and other symptoms
For more severe cases of PAD, artery catheterization or surgical treatment may be required to clear blockages and restore normal blood flow. Some of the most commonly used procedures for PAD include:
Angioplasty – During this procedure, a catheter with a balloon or other device on the end is inserted into a blocked artery. The balloon is then inflated, which pushes the plaque outward against the wall of the artery. This widens the artery and restores blood flow.
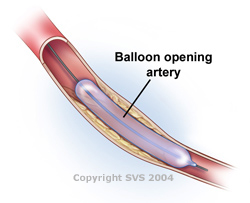
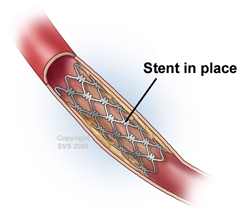
Stents – A stent (a small mesh tube) may be placed in the artery during angioplasty. A stent helps keep the artery open after angioplasty is done. Some stents are coated with medicine to help prevent blockages in the artery.
Bypass Grafting – For this surgery, your doctor uses a blood vessel from another part of your body or a man-made synthetic hose / tube to re-route or detour the blood around the area of blockage. This surgery doesn’t cure PAD, but it tends increase blood flow to the affected limb. This will help to diminish the chances of further complications related to the disease.
For a consultation to assess your PAD or to be screened for PAD, call our Vascular Center at (512) 339-9100.